I was blessed this week to have the opportunity to attend a Summit to address Alberta Insurance Reform. As you can imagine with different professionals who passionately believe in their personal profession, vibrant discussions were held.
How Many People Fully Recover After a Motor Vehicle Collision Injury Was Sustained?
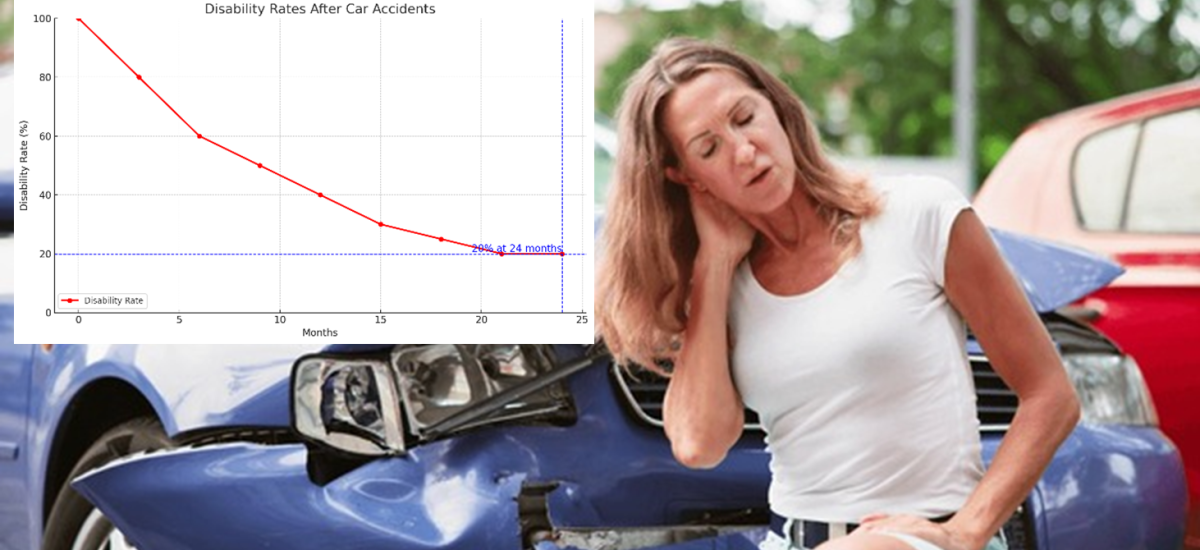
One of the debates focusses on the approximately 20-30% of people (internationally across different jurisdictions) who fail to fully recover, two-years following a motor vehicle collision. Of note is that 6- to 12- months post-injury, 50% have not fully recovered (1, 2). We have covered this in a previous post. It is common knowledge that not all people recover. Just the same as not all sporting injuries fully recover.
Our Current Tort System Management of Non-Recovery
On one hand, our current system provides the possibility of a negotiated cash settlement between a lawyer representing an injured person and the insurance company providing the insurance. In theory, this money provides for future care and an established amount for pain and suffering that reflects the fact (as established by medical professionals and agreed to by both parties) that person has not returned to their prior state of health and wellbeing. This cash then allows that person to pursue further treatment as required, which is provided through the ‘private system’ by the health care practitioner of their choice. In my experience, having not known another system, this works well, with many patients following up heir health care provider of choice when pain flares occur. We would see the same situation occur in a sporting situation when a person sustains a head injury or hip/knee pathology that results in an inability to pursue their recreation and need for ongoing care to address their now residual symptoms.
An Alternative Viewpoint
Now, on the other hand, there was strong support to abolish this payment. The group of people advocating for such were quite strong in their opinions suggesting that the money is not going to care, but other lifestyle initiatives. The thought is, that removing this a) saves money and b) prevents unnecessary focus on poor health behaviours which are reinforced by cash settlements. The other associated ‘selling point’ of this argument is that the money saved from cash settlements can be reinvested into ‘more care’, especially ‘early care’. Now, on the face of it, that sounds just grand, but as The Streets have sung: A Grand Don’t Come for Free.
But There Is $50K Available for Treatment, Surely That Is Enough for Any Injury…
It is common knowledge, that although $50,000 is currently available for treatment under Section B, very, very few (if any) people have access to this amount, as IMEs are ordered if people don’t improve, which results in the person having their care discontinued. This then results in lawyer assistance to navigate their rights, given that they are still having care for ongoing symptoms. Thus, removing cash settlements would appear to then require an assurance that IMEs would not be used to prevent people accessing the $50K available for treatment.
A Question or Two
Now, being a nerd and not being afraid to speak my mind (which can be dangerous as many of you know!), I asked a tough question – given that more early care is associated with worse health outcomes (1-3), and this data is robust and established in high levels of evidence (systematic reviews), how does ‘more’ care help the 20%?
Again, I asked: What are we going to do with those who don’t recover at 2 years? Now, I know blank stares, but I’ve never seen so many blank, blank looks – I was approached later with the suggestion that: well, more care will fix those people. Again, I am a nerd, but I don’t know any data that suggests more care reduces the volume of people having persistent symptoms after 2 years – that’s just the literature speaking. I do know that one treatment – stress inoculation training reduces transition to chronicity (4), but that’s the best we have in the ‘prevention’ of chronic pain literature.
Secondly, when asked if insurers could guarantee that the care of injured Albertans would not be lessened by any proposed changes, no answers were forthcoming. Now, that is because some of the proposed changes in different jurisdictions advocate for an end of treatment after 25 treatments (within 12 weeks) or after a restricted treatment $ amount at 6 months.
Thus, again, I ask the question, what about those that don’t fully recover within that time frame – do they hit Alberta Health Services for treatment of their persistent pain, remembering that there is roughly a 2-year waitlist for admission into the Calgary Chronic Pain Centre. Or do they hit urgent care when they have a pain flare, or do they access opioids? Where do these people go for ongoing treatment? I have to admit I do not know the answers. But I do see unintended consequences of removing cash settlements. I also see that the currently framed argument justifying ‘more care’ rather than ‘cash’ is flawed and inconsistent with scientifically accepted evidence-based literature. But don’t let that get in the way of a good story 😉
I truly hope that evidence for consumer’s best health outcomes outweighs ideology. Time will tell. Until next time – please, please, please complete the government survey to share your opinion on Alberta Insurance Reform.
References:
- Carroll, L.J., L.W. Holm, S. Hogg-Johnson, et al. Course and prognostic factors for neck pain in whiplash-associated disorders (WAD): results of the Bone and Joint Decade 2000-2010 Task Force on Neck Pain and Its Associated Disorders. Spine 2008; 33(4 Suppl):S83-92.
- Shearer, H.M., L. Carroll, P. Cote, et al. The course and factors associated with recovery of whiplash-associated disorders: an updated systematic review by the Ontario protocol for traffic injury management (OPTIMa) collaboration. European Journal of Physiotherapy 2020; 23(5):279-294.
- Cote, P., S. Hogg-Johnson, J.D. Cassidy, et al. Early aggressive care and delayed recovery from whiplash: isolated finding or reproducible result? Arthritis Rheum 2007; 57(5):861-8.
- Sterling, M., R. Smeets, G. Keijzers, et al. Physiotherapist-delivered stress inoculation training integrated with exercise versus physiotherapy exercise alone for acute whiplash-associated disorder (StressModex): a randomised controlled trial of a combined psychological/physical intervention. Br J Sports Med 2019.