It is always a pleasure to get notification that a project you are working on has been accepted for publication. That happened this week when the European Journal of Physiotherapy green-lighted the publication of a study where we investigated the role of platelet-rich plasma in the treatment of people with chronic whiplash symptoms that had previously responded to a diagnostic facet joint block. We had previously presented this as a poster at an international conference to get some feedback, but it is gratifying to see the full manuscript accepted for publication. It gives you a warm fuzzy feeling just as Grant Lee Buffalo provided to all the College kids in 1993.
What Is Platelet-Rich Plasma?
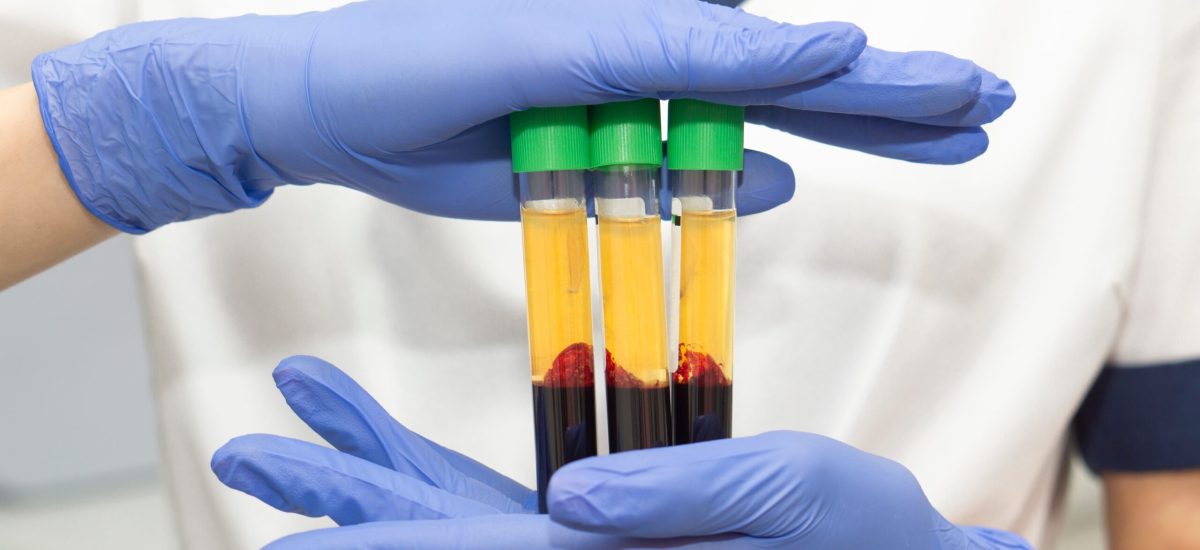
Platelet-rich plasma or PRP as it is commonly known, is as the name describes, a concentrated sample of platelets contained within plasma obtained from a person’s blood sample. The blood is spun rapidly in a centrifuge to concentrate the platelets in the plasma before this is injected with X-ray or ultrasound guidance into the person requesting such.
What are the possible benefits of PRP?
Platelets are known for their healing abilities – assisting with clotting, but also possessing growth factors to facilitate healing. There is also an anti-inflammatory component that assists with pain relief associated with inflammation.
Is It Safe? I Hear the Procedure is Painful…
The best evidence we have for PRP is its safety. In the 3 studies we have published, safety has not been an issue. No adverse events have been reported. Now, that is not to say that it isn’t painful. Think of a bruise. It is a couple of days before you actively increase movement and push your limits to the maximum in the presence of a bruise. Similarly, following PRP, there are 2 days that require relative rest compared to pursuing usual activities, and then approximately 7-10 days where activity modification is required (e.g. less strenuous activity). However, by week 3 as the healing process takes hold, people are encouraged to resume normal activities and progressively strengthen the areas in and around the injected site to improve functional ability.
What Did This Study Tell Us About PRP?
Firstly, this was the first trial investigating PRP in the facet joints of the neck, where we randomized individuals to different post-PRP care after the injection (physiotherapy or ‘usual’ care = booklet with advice and home exercises + access to a doctor) and staggered their rehabilitation to help validate the results. Other studies involved case reports or followed a series of patients over time, which generally results in an over-inflation of the benefits of an intervention.
What Did Physiotherapy Involve?
An experienced post-graduate trained physiotherapist provided pragmatic care – meaning that if you tested weak or had poor endurance of your neck and trunk muscles, you received strength and/or endurance exercises (progressively guided to achieve age and sex matched normative data); if you were restricted in your mobility, you received manual therapy and exercises to address such; if you weren’t physically active enough, you were told to move as per population-based guidelines. General advice and education was provided, but no specific pain neuroscience education was provided.
One interesting aspect from this study, is that those who did not receive physiotherapy, but had a take home booklet, actually performed more home exercises – they were more diligent. Maybe that’s why there were no group differences in outcomes after the study finished.
What Was Measured?
We measured each person’s daily pain and confidence in performing activities (despite having neck pain) for the six weeks after completing their care. This was a big undertaking for each person in the study. Thus, we did lose one person for the final measurements, which is understandable, given the length of the study. We then reviewed progress 3 months later to see if improvements were retained.
What Was the Take-Away Message?
As above, there were no adverse events reported. Also, each person receiving PRP reported significant benefit after treatment (physiotherapy or ‘usual’ care), with no difference in outcomes (pain or confidence in performing activities) reported between groups. Outcomes were maintained 3 months later. However, the study wasn’t strong enough to test differences between groups. But the difference between groups was so small, that future studies would need to enroll a lot more participants in the study to determine if a group difference did in fact exist.
The most interesting finding is that for 4 of the 6 participants, their pain reduced significantly to such an extent that they did not see any further reduction of strength of that magnitude in the remainder of the study. This suggests that PRP was imparting an anti-inflammatory effect rather than a regenerative effect. Thus, the pain arising from the facet joints post-whiplash injury might be inflammatory in nature, and PRP might be able to assist with such. This opens up possibilities for future biological procedures that may assist those following a whiplash injury.
However, lots of questions remain that require answering which we are attempting to sort our way through – How many doses of PRP do you need? What concentration is optimal for different aged people? Is leukocyte rich or poor concentrations preferred for a particular person? What is the optimal inclusion criteria? As we get the answers to these questions, personalized pain medicine then becomes possible.
Reference:
Smith A, Gupta A, Stone J, Habberfield J, Schneider G. The Efficacy of Multimodal Physiotherapy and Usual Care in Chronic Whiplash-Associated Disorders with Facet-Mediated Pain Undergoing Platelet Rich Plasma (PRP) treatment: A Series of Single Case Experimental Designs (SCEDs). Eur J Physio 2024 (Accepted for publication March 4, 2024)