I have blogged on this previously, but a very hot topic at the World Congress of Pain has involved the topic and appropriate use of the terminology involving Central Sensitization (CS). In essence, this term has been abused by many over the years. The definition very clearly relates to a physiological response within the central nervous system. However, it has been co-opted by clinicians to help provide an explanation for ‘unexplained pain’. In essence, this needs to stop. Clinicians should not be using this word – it is not a diagnosis. It is an underlying mechanism observed in animal studies that we cannot measure in humans. So what is the alternative to describe humans with a) widespread pain not localized to a single tissue – simply describe this as: widespread pain without an evident nociceptive focus; b) local pain, but widespread reduced sensitivity to evoked stimuli such as pressure, pain or electrical applications – well, describe that without confounding these test results as a mechanism to explain the pain behaviour. We really do not know what mechanisms are driving these test results.
Now that brings me to my presentation at Congress – on Offset Analgesia – an attempt to quantify descending pain modulation. And of course, my poster was full of the words CS – as in, this may be associated with outcomes in chronic whiplash associated disorders (WAD). So far so good. The next assumption fell short of negating the above criticisms!!! Essentially, we are unsure what underlying mechanisms drive CS in WAD.
Offset Analgesia – What Did We Find?
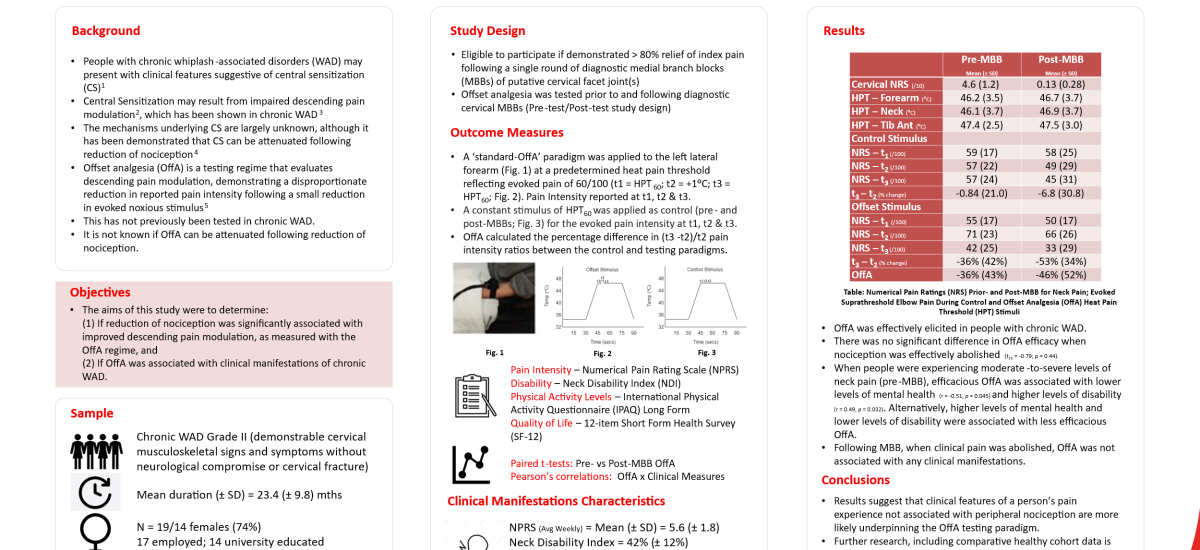
We investigated 19 people with chronic WAD of 2 years duration with moderate to severe pain and disability. They completed questionnaires and performed tests generally associated with features suggestive of CS. They also underwent an offset analgesia paradigm. This is a neat test, whereby a person receives a heat stimulus for 5 seconds that results in 6/10 pain. Then the temperature increases 1⁰C, before reducing 1⁰C. Interestingly, a healthy person demonstrates a disproportionate reduction in pain when this mild reduction occurs. Our participants recorded 36% less pain than that experienced prior to the temperature increase. This is a standard response, indicating that there were no deficits observed in the whiplash cohort – that is good for the people involved – but doesn’t help us understand people with persistent pain. Especially when these findings were not related to other clinical features.
The second part of this study involved us re-testing this paradigm when the pain was abolished – i.e. after a local anaesthetic blockade to the little facet joints in the neck. Of interest, is that there was a 10% increase in response, but this was not statistically significant. Thus, this tells us that offset analgesia is not likely affected by underlying sources of tissue pathology. We have much more to this story to share yet, so I’ll leave this here for the time being…more fun to be had tomorrow when I have the privilege to listen to two giants of the pain field who received the Nobel prize for medicine. Inspiring!