Here are a few stats for those interested in such. For those that aren’t, then enjoy the figure below. A picture tells a 1000 stories, so maybe that works for you. I was hit with a query last week from a ‘third party’ regarding the non-recovery of a person seeking further evaluation of their persistent pain that reportedly originated from a motor vehicle collision (MVC) approximately 18 months ago. Some doubt was cast on the veracity of the person’s complaints ‘given that everyone heals by 90 days’. That’s a big statement I thought to myself. We don’t question sports people who take 12 months to recover from knee injuries and attend rehab for that period of time. Now maybe this ‘third party’ was influenced by Amy Winehouse whereby she wouldn’t “go, go, go” to rehab after repetitively saying “no, no, no”. But in this situation, the injured person had attended rehab and was diligent with such. Now, thankfully the ‘third party’ making these assertions was willing to listen. As Thomas Dolby sang back in 1982, I blinded them with science ->
What does research tell us about recovery following injuries sustained in motor vehicle collisions?
As our title suggests, not everyone recovers in the same time period. A series of systematic reviews all report the same – approximately 50% of those injured in a motor vehicle collision continue to report symptoms at 6- to 12- months, with studies with longer follow-up periods reporting that approximately 20-30% of people continue to report symptoms two-years post-injury. The systematic reviews are summarizing all studies investigating prognosis, and thus we are confident that these figures are representative across different jurisdictions internationally. And not everyone recovers the same as this adaptation demonstrates. In this modelling study, for those that don’t recover, some have mild self-reported pain-associated disability and fewer (16%) demonstrate chronic-severe symptoms.
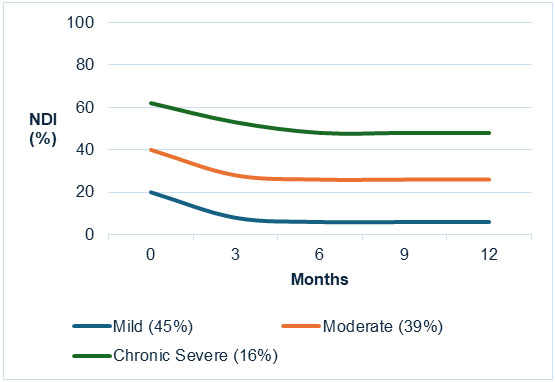
Adapted from Sterling et al. (1)
Can you predict if someone is not going to recover?
Now there are some very clever researchers that have approached this in different ways – predominantly due to their access to different recovery data. Some have looked at clinical data, some at hospital data, some at insurance data. Given that I primarily practice within a clinic, let’s look at some clinical data that has been validated (2). That is important, as you can derive a model to predict who might or might not recover based on historical data (3), but then testing that data prospectively in another sample allows us to validate the veracity of that model, and that’s what one very, very clever group of extraordinary researchers did (and yep, I did work alongside them, so I can attest to their wonderfulness 😉). They were able to demonstrate that initial high levels of pain-associated disability (a score > 19/50 on the Neck Disability Index) AND high stress levels ( PDS hyperarousal score > 5) AND age > 34 years predicted ongoing moderate-severe symptoms at 6-months. This was highly predictive (91% positive predictive value). Whilst the contrary showed that those with scores < 17 on the NDI and aged < 36 years were predicted to have a full recovery (again, highly predictive = 80%). Those that didn’t fit either of these pathways were neither predicted to have full recovery or moderate to severe symptoms at 6 months.
What about predicting ‘general recovery’?
Maybe clinicians don’t have access to the NDI and PDS – although any person serious in helping people with injuries sustained in motor vehicle collisions should!!! Well, another researcher encased in wonderfulness, Professor David Walton has historically updated the literature on features predictive of poor recovery (4). Using some methodologically rigorous criteria, the following variables predict an inability to fully recover by 6-months: initial presentation of high neck pain intensity (> 5.5/10), initial presentation of higher NDI score (>15), initial presence of headache, initial presentation of neck pain vs. no neck pain, pain catastrophizing, presence of low back pain, higher levels of WAD grading (e.g. Grade 2 or 3 vs 0 or 1), female sex, less than postsecondary education, no seatbelt used or pre-collision history of neck pain.
Of interest, is most of these relate to symptoms reported by the injured person, and not the severity of motor vehicle collision sustained. Thus, clinicians need to be aware of these factors when providing initial evaluation of people injured in motor vehicle collisions. With constant monitoring of outcomes such as pain, disability and stress, changes over time can be appreciated. If no change is being observed within 3-months, then referral for further evaluation is recommended. As we’ve previously reported, further management outside of traditional conservative management would be recommended.
References:
- Sterling, M., J. Hendrikz, and J. Kenardy Compensation claim lodgement and health outcome developmental trajectories following whiplash injury: A prospective study. Pain 2010; 150(1):22-8.
- Ritchie, C., J. Hendrikz, G. Jull, et al. External validation of a clinical prediction rule to predict full recovery and ongoing moderate/severe disability following acute whiplash injury. The Journal of orthopaedic and sports physical therapy 2015; 45(4):242-250.
- Ritchie, C., J. Hendrikz, J. Kenardy, et al. Derivation of a clinical prediction rule to identify both chronic moderate/severe disability and full recovery following whiplash injury. Pain 2013; 154(10):2198-206.
- Walton, D.M., J.C. Macdermid, A.A. Giorgianni, et al. Risk factors for persistent problems following acute whiplash injury: update of a systematic review and meta-analysis. J Orthop Sports Phys Ther 2013; 43(2):31-43.





