Well, when it rains, it pours it seems. Eddie Rabbitt, as I do, loved a rainy night back in the ‘80s. However, being a nerd, I also love getting news of an accepted publication. After a publication for PRP for neck pain was recently accepted, it was a pleasure to hear that a pilot project of ours investigating PRP for low back pain was also accepted for publication. The full publication can be found here.
What Is Low Back Pain of Likely Disc Origin?
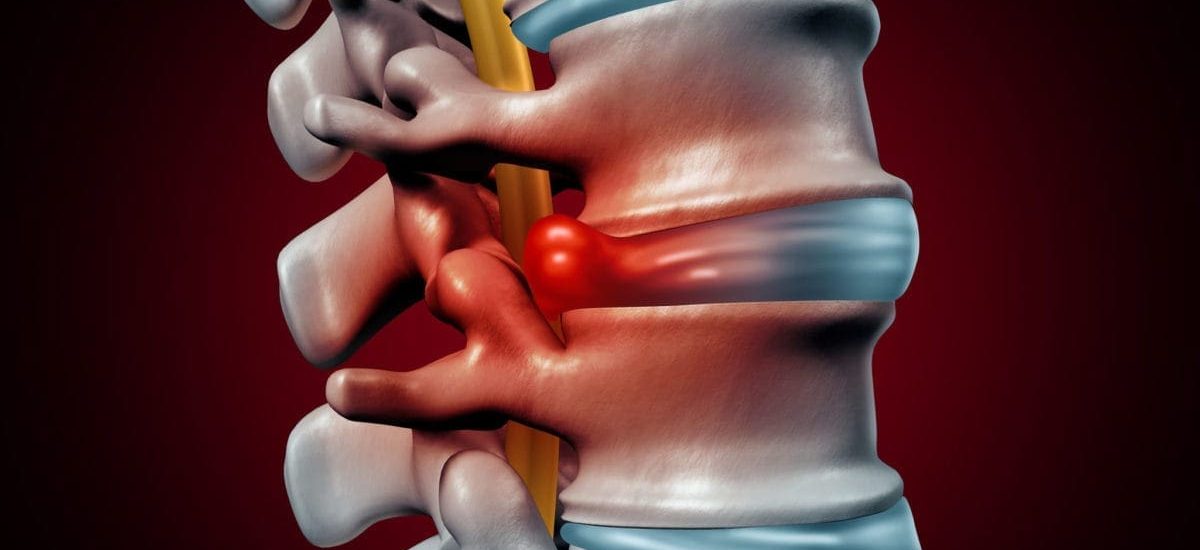
Many structures in your back can be a source of pain. The most common of these is the disc, which is an amazing and resilient structure that helps to transfer load in the low back. It consists of an outer fibrous structure (annulus fibrosus) that houses an inner nucleus gel. As with any structure, it can be injured. Quiet possibly many people have heard of disc herniations whereby the inner nucleus herniates through the outer annulus, which can then result in an irritation of one of the nerves that travels into the leg. However, more commonly, and generally in younger people the nucleus can push outwards into a tear within the annulus without pushing on any nerves. This is termed internal disc disruption (IDD).
How Is Internal Disc Disruption Diagnosed?
Internal disc disruption is a challenge to diagnose accurately. The reference/gold standard test involves a needle puncture of the disc with a pressure-controlled injection of dye to determine if the person’s familiar pain is reproduced. As most of you would likely know, this is painful in any person, so a ‘negative’ response is required when a needle reproduces an adjacent disc. Not fun I hear most people say. That’s true. Different researchers have investigated other methods of detecting IDD presence. An MRI scan has some utility in predicting the presence of IDD. A ‘high intensity zone’ (speak to a radiologist to help with that determination) and a generally looking ‘black’ disc point to the presence of IDD.
Can You Treat IDD?
Internal disc disruption is hard to treat! Sure, if a person has deteriorating neurological status (persistent numbness, loss of muscle power and loss of reflexes) then surgery might be an option (after you discuss this with a surgeon). Otherwise, not many treatments exist that demonstrate long term reduction of low back pain for pain of likely disc origin. That’s where our study came in.
Rather than put a needle into the disc, we chose people who presented with low back pain (without leg pain) that presented with the above MRI findings and whose pain was not relieved with injection of the surrounding facet joints. We then injected platelet-rich plasma (PRP) into the epidural space.
What Is Platelet-Rich Plasma?
Platelet-rich plasma or PRP as it is commonly known, is as the name describes, a concentrated sample of platelets contained within plasma obtained from a person’s blood sample. The blood is spun rapidly in a centrifuge to concentrate the platelets in the plasma before this is injected with X-ray or ultrasound guidance into the person requesting such.
Why PRP You may ask…
Platelets are known for their healing abilities – assisting with clotting, but also possessing growth factors to facilitate healing. There is also an anti-inflammatory component that assists with pain relief associated with inflammation.
Does PRP Improve Pain of Likely Disc Origin?
Yes…and no. This was a small pilot study with 11 people. Eight people reported significant pain relief 12-months later. The average pain response 12-months post-procedure was a 35-40% improvement. Four people reported > 50% relief of pain. No complications were reported.
Thus, this study adds to data suggesting that PRP delivered for spinal pain is safe. However, we can’t pick out those patients who will or won’t respond, which makes this a little tricky when recommending it to patients. But for those who it works for, PRP provides sustainable pain relief with a low side effect profile. Thus, the journey continues…
Reference:
Playfair, Smith A, Burnham R. An evaluation of the effectiveness of platelet rich plasma epidural injections for low back pain suspected to be of disc origin – A pilot study with one-year follow-up. Int Pain Med. (2024):Vol 3(2);100403